Many advancements in medicine begin with a single, well-informed decision. In the past, these decisions were made by experienced clinicians relying on training, intuition, and experience. Today, doctors operate in a far more complex environment with high patient volumes and painful administrative demands. Their decision making needs to be faster and data driven. The use of generative AI for clinical decision making is alleviating the stress that comes with high patient volumes.
Making the best clinical choices can't rely on experience or intuition alone. They need to be backed by data-rich insights. Artificial intelligence for clinical decision-making is emerging as that critical ally, helping healthcare organizations transform information-overload into confident, timely, and consistent patient care.
Why AI for clinical decision-making matters?
To understand this in the right context, consider the number of daily decisions in a typical clinic: triaging patients, prioritizing cases, reviewing test results, and choosing follow-up care. Even the best doctors are limited by time and cognitive overload. What if you could support your team with data-driven insights and automated workflows?
- Faster diagnostics: AI spots patterns in patient data, imaging, and lab reports faster than manual review.
- Personalized care: Algorithms identify patient-specific risk factors or responses to treatment.
- Reduced errors: AI cross-references vast datasets and protocols to minimize oversights.
- Operational efficiency: Automation takes care of repetitive tasks like documentation or appointment reminders.
How is AI helping doctors with clinical decision-making?
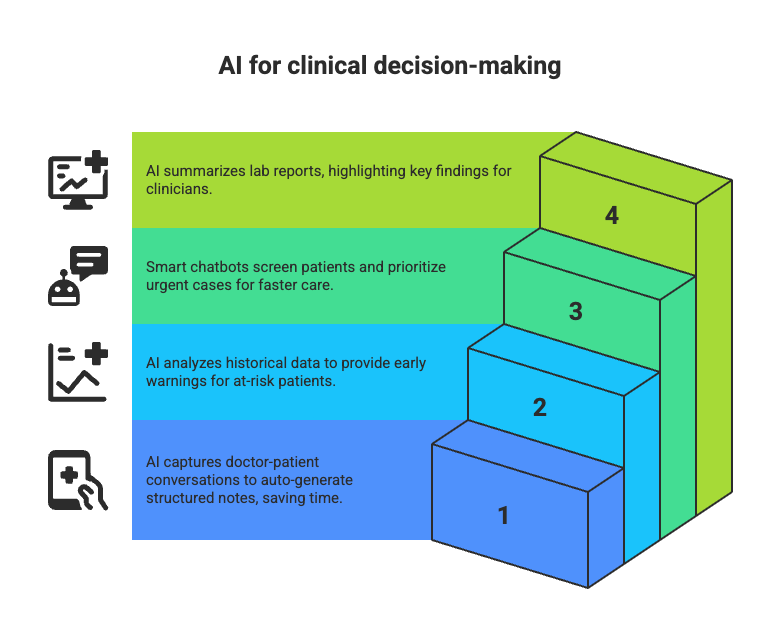
AI is quietly improving everyday workflows, right from reducing manual effort, speeding up decisions to helping clinicians focus more on care. Even smaller clinics can start using AI in a few, targeted areas:
- Clinical note generation: AI can capture doctor-patient conversations and auto-generate structured clinical notes, freeing doctors and their assistants from hours of typing.
- Risk prediction tools: By analyzing historical data, AI models offer early warnings for patients at risk of complications, readmission, or deterioration.
- Automated triage systems: Smart chatbots can ask screening questions and flag urgent cases, getting the right patients seen sooner.
- Lab report summarization: Instead of reading every detail, clinicians get concise AI-powered summaries highlighting key findings.
How to get started with AI for clinical decision-making?
Implementing AI in clinical decision-making is a sure way to reduce doctor stress and improve accuracy. Even a small, targeted rollout in the right area can show results within weeks. Here’s a simple roadmap to begin your AI journey:
Step 1: Identify high-friction areas
Begin by asking: Where are the biggest delays or frustrations for your doctors? Is it in reviewing lab reports? Writing up clinical notes? Spotting at-risk patients in time?
By focusing on one or two pain points, especially those that are repetitive or time-consuming, you’ll find natural entry points for automation and assistance. These areas are often where AI in clinical decision-making delivers the highest impact with minimal disruption.
Step 2: Start with a focused pilot
AI doesn’t have to touch every part of your clinic on day one. In fact, it shouldn’t. Start small. For example, pilot AI for lab report summarization, clinical note generation, or automated triage.
These are high-frequency tasks where even a small improvement translates into big time savings, and they don’t require deep integration with your EMR right away.
Step 3: Choose an AI implementation partner with real healthcare deployment experience
Not all AI vendors understand the clinical world. Look for teams with proven case studies, real-world deployments, and a track record in regulated healthcare environments.
Gen AI development companies like GoML, for instance, have deployed systems that are actively used by hospitals and clinics across specialties.
Step 4: Involve your clinical staff early
The success of AI in clinical decision-making depends on trust and usability. When clinicians see that the system offers recommendations, not rigid decisions, they’re more likely to adopt and engage.
Step 5: Track the impact and adjust
Finally, don’t “set and forget” your AI system. Measure what matters:
- Are clinical decisions happening faster?
- Is the documentation workload lighter?
- Are patients being triaged more accurately?
Track improvements in speed, accuracy, and satisfaction. Then tweak your approach based on what’s working and what’s not.
By following this phased approach, clinics of any size can begin using AI in clinical decision-making to improve care quality, reduce manual burden, and deliver faster, more consistent outcomes.
What are some real-world applications of AI in clinical decision-making?
Improving clinical decision making with AI
Atria’s hospitals turned to GoML to implement AI for hospitals to assist with daily decisions. The results speak for themselves:
- Clinical decision-making improved by 80%. Doctors received AI-powered recommendations during consultations, which led to more accurate diagnoses and better treatment plans.
- The system analyzed patient data across EHRs, test results, and medical histories in seconds, something impossible before.
- Automated triage and early warning systems enabled staff to spot at-risk patients and intervene sooner.
Turbocharging retinal disease detection
An eye-care clinic needed help triaging thousands of patients for retinal conditions. GoML delivered an AI solution for retinal disease detection that:
- Increased triage speed by 85%, ensuring urgent cases were fast-tracked to specialists.
- Automatically flagged subtle patterns in imaging data, patterns easy for the human eye to miss when faced with volume.
Not only did patient wait times shrink, but ophthalmologists had more time for complex cases, boosting both efficiency and outcomes.
Predicting and preventing patient health risks
Atria needed a better way to anticipate clinical deterioration and reduce avoidable emergencies. GoML upgraded their existing systems with an AI-powered health risk prediction system that could analyze patient data in real time, flagging individuals at higher risk for complications before symptoms became critical.
This helped Atria:
- Improve risk prediction accuracy by 50%, giving staff a clearer picture of which patients needed proactive care.
- Act sooner, with early alerts enabling faster interventions and better outcomes.
- Reduce emergency escalations and lower the burden on frontline workers.
What used to take hours of manual data review now happened in seconds, turning clinical surveillance into preventive action.
AI for clinical decision making doesn’t have to be disruptive to your existing workflow. Simple, targeted changes can free up your time and safeguard patient care.
Ready to take the next step? GoML is a leading Gen AI development company that helps you implement cutting-edge solutions to move your clinical strategy forward faster, smarter, and at scale. If you’re serious about improving efficiency for your clinic, reach out to us today.